
Neuro-ophthalmology is a subspecialty of both neurology and ophthalmology that deals with diseases and disorders affecting the visual pathways and the eye movements controlled by the brain. Neuroophthalmologists are experts in diagnosing and managing conditions such as optic neuropathies, cranial nerve palsies, and visual disturbances related to neurological disorders like multiple sclerosis. They utilize specialized techniques and equipment to assess visual function, perform detailed eye examinations, and interpret imaging studies of the brain and optic nerves.
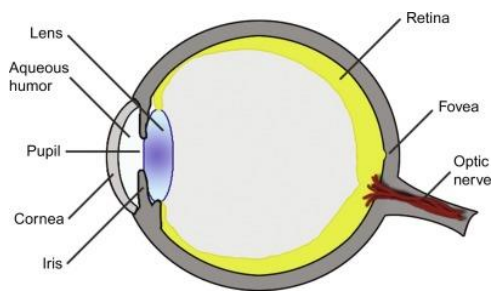
1. Diagnosing Optic Nerve Disorders: Neuro-ophthalmologists are skilled at diagnosing conditions that affect the optic nerve, such as optic neuritis or optic neuropathy. They use tools like optical coherence tomography (OCT) and visual field testing to assess the structure and function of the optic nerve.
2. Managing Double Vision: Conditions causing double vision (diplopia) often have neurologic origins. Neuro-ophthalmologists can pinpoint the underlying cause and recommend treatments, including prisms, eye exercises, or surgery when necessary.
3. Identifying Visual Field Defects: Neuro-ophthalmologists can detect and quantify visual field defects that result from neurological conditions like strokes, tumors, or intracranial pressure changes. This information is crucial for diagnosis and management.
4. Assessing Pupillary Abnormalities: Pupillary abnormalities can be indicative of various neurological disorders. Neuro-ophthalmologists can evaluate these abnormalities and contribute to the diagnosis of conditions such as Horner’s syndrome or Adie’s tonic pupil.
Neurologists are experts in diagnosing and managing neurological disorders that may have visual manifestations. These two specialties complement each other in several ways:
1. Neurological Investigations: Neurologists perform comprehensive neurological assessments to identify the root cause of visual disturbances. This often includes brain imaging (e.g., MRI or CT scans) to look for structural abnormalities that may affect the visual system.
2. Coordinating Care: Neurologists act as central coordinators when a patient presents with complex neurological and ophthalmological issues. They ensure that all aspects of a patient’s care are integrated and well-managed.
3. Managing Systemic Diseases: Neurologists treat systemic diseases that can impact the visual system, such as diabetes, hypertension, and autoimmune disorders. Effective management of these conditions can help prevent or minimize vision-related complications.
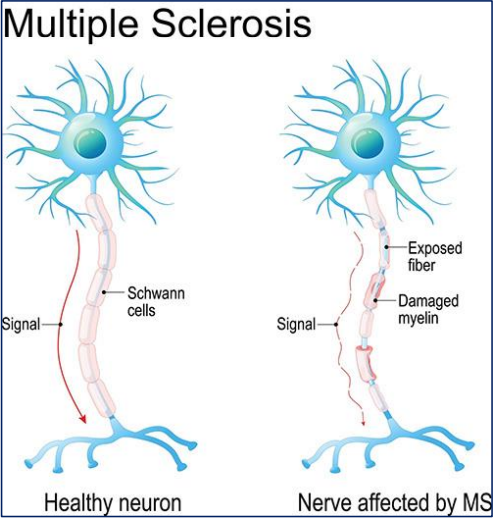
4. Treating Neurological Disorders: Neurologists play a crucial role in treating neurological conditions like multiple sclerosis, strokes, and brain tumors that can affect the visual system. Their interventions often complement the treatments provided by neuro-ophthalmologists.
5. Medication Management: Neurologists can prescribe medications to alleviate symptoms of neurological conditions that impact vision, such as headache management for migraines or immunosuppressants for optic neuritis related to autoimmune disorders.
Multiple sclerosis (MS) is a prime example of a condition where the collaboration between neurologists and neuro-ophthalmologists is essential. MS can cause optic neuritis, leading to vision impairment. Neuro-ophthalmologists diagnose and monitor optic neuritis, while neurologists manage the underlying MS, ensuring the patient receives comprehensive care.
The collaboration between neurologists and neuroophthalmologists is indispensable for providing comprehensive care to patients with visual health issues. Together, they bring a multidisciplinary approach to diagnose and manage complex conditions that affect the visual system. By working in tandem, these specialists ensure that patients receive the best possible care, addressing not only the eye-related symptoms but also the underlying neurological causes, ultimately preserving and enhancing the gift of sight.
Copyright 2021 www.northwestneurologymi.com. All rights reserved.